Receiving a prostate cancer diagnosis can be an overwhelming experience. It’s natural to feel a whirlwind of emotions – anxiety, confusion, and fear. But alongside these emotions, there’s something critically important: hope. Understanding your diagnosis, what lies ahead, and the resources available to you can make all the difference in how you navigate this journey.
The good news is that with early detection, prostate cancer is highly treatable, and even advanced stages can be managed effectively. Let’s walk through what you can expect after a diagnosis and how to take the next steps with clarity and confidence.
Understanding prostate cancer diagnosis
Early vs. advanced diagnosis
Prostate cancer is generally classified into two main categories:
- Early diagnosis: This is often achieved through proactive PSA (prostate-specific antigen) screening. In these cases, the cancer is confined to the prostate, making it highly treatable. Options such as surgery or radiation are typically very effective at this stage. Detecting prostate cancer early provides a wider range of treatment options and increases the likelihood of successful outcomes.
- Advanced diagnosis: This includes cancer that has spread just outside the prostate (locally advanced) or to more distant areas like the bones or lymph nodes (metastatic cancer). While advanced prostate cancer may not be curable, treatments can significantly improve quality of life and help manage the disease effectively. This stage often requires a more comprehensive approach involving a team of specialists to address complex care needs.
More on the PSA test
The PSA test is often the first step in detecting prostate cancer. PSA, a protein produced by the prostate, is present in small amounts in every man’s bloodstream. However, elevated PSA levels can indicate several conditions, including prostate enlargement, infection, inflammation or cancer. It’s important to understand that the PSA test alone doesn’t confirm cancer but rather signals the need for further investigation. Additional tests, such as MRI scans or biopsy, can then determine whether cancer is present and, if so, its stage and aggressiveness.
For men seeking immediate results, private clinics can often provide rapid testing and assessments, allowing for quicker decision-making. While the PSA test isn’t definitive, it’s a crucial first step for identifying those who may need further evaluation. Men who are concerned about their PSA levels should discuss their results thoroughly with their healthcare provider to understand what the numbers mean in the context of their overall health.
The role of screening
Screening plays a vital role, especially for high-risk groups. Black men and those with a family history of prostate cancer are 2-3 times more likely to develop the disease. For these groups, routine PSA testing is essential for early detection, where treatment success rates are significantly higher.
However, for men over 80, routine testing is often avoided due to the risks potentially outweighing the benefits. It is essential to weigh the pros and cons of regular screening, and this decision should be made collaboratively between patients and their doctors.
Key statistics
The average age at diagnosis is the mid-60s, and the risk increases with age. Globally, prostate cancer is the second most common cancer in men, emphasising the importance of awareness and regular health check-ups. It’s estimated that one in eight men will be diagnosed with prostate cancer at some point in their lives. Knowing this statistic highlights the importance of regular screening and proactive health measures for men of all ages.
Steps before prostate cancer diagnosis
Following a raised PSA
After a raised PSA test, an MRI scan is done to determine if a prostate biopsy is necessary.
- MRI scans: These provide detailed images of the prostate and surrounding areas, identifying whether a biopsy is needed to investigate if cancer is present. Any abnormality seen within the prostate is classified using the PIRADS or Likert system, which scores abnormalities from 1 to 5, with higher scores indicating greater suspicion of cancer. An MRI scan not only helps determine the risk of a cancer being present but also identifies its location and assesses whether it has grown beyond the prostate, influencing the course of treatment.
- Biopsies: A biopsy is the only definitive way of confirming a prostate cancer diagnosis. This involves taking small samples of prostate tissue, usually guided by ultrasound and using the MRI scan as a road map. Pathology results reveal the aggressiveness of the tumour, using the Gleason grading system, which ranges from 6 (slow growing), through Gleason 7 (intermediate risk) to Gleason 8 – 10 (aggressive). These results, combined with PSA levels and MRI findings, form the basis for creating a tailored treatment plan. In some cases, multiple biopsies may be required to provide a comprehensive understanding of the tumour.
Treatment discussions
Once the cancer’s specifics are clear, your medical team will discuss treatment options. Every man’s journey is unique, and the choice of treatment will depend on factors such as the cancer’s stage, your age, overall health, and personal preferences. Understanding the pros and cons of each option can help you make informed choices that align with your goals and values.
- Active surveillance: For slow-growing (usually Gleason 6) localised cancers, regular monitoring through PSA tests, MRIs, and occasional biopsies is usually recommended. This approach avoids or delays definitive treatment unless or until there are signs of progression. Active surveillance allows many men to maintain their quality of life without undergoing unnecessary procedures.
- Focal therapy: This minimally invasive option targets only the cancerous half of the prostate, preserving as much healthy tissue as possible and reducing side effects. It’s an emerging treatment that can be an excellent choice for men with small, localised tumours. However, follow-up prostate biopsies typically reveal residual cancer in 20–30% of men within a year of focal therapy.
- Radiotherapy: This uses high-energy radiation to destroy cancer cells. Options include external beam radiation or brachytherapy, where radioactive seeds are implanted in the prostate. Radiotherapy may require multiple sessions over several weeks, but advancements in technology have made it more precise and less protracted.
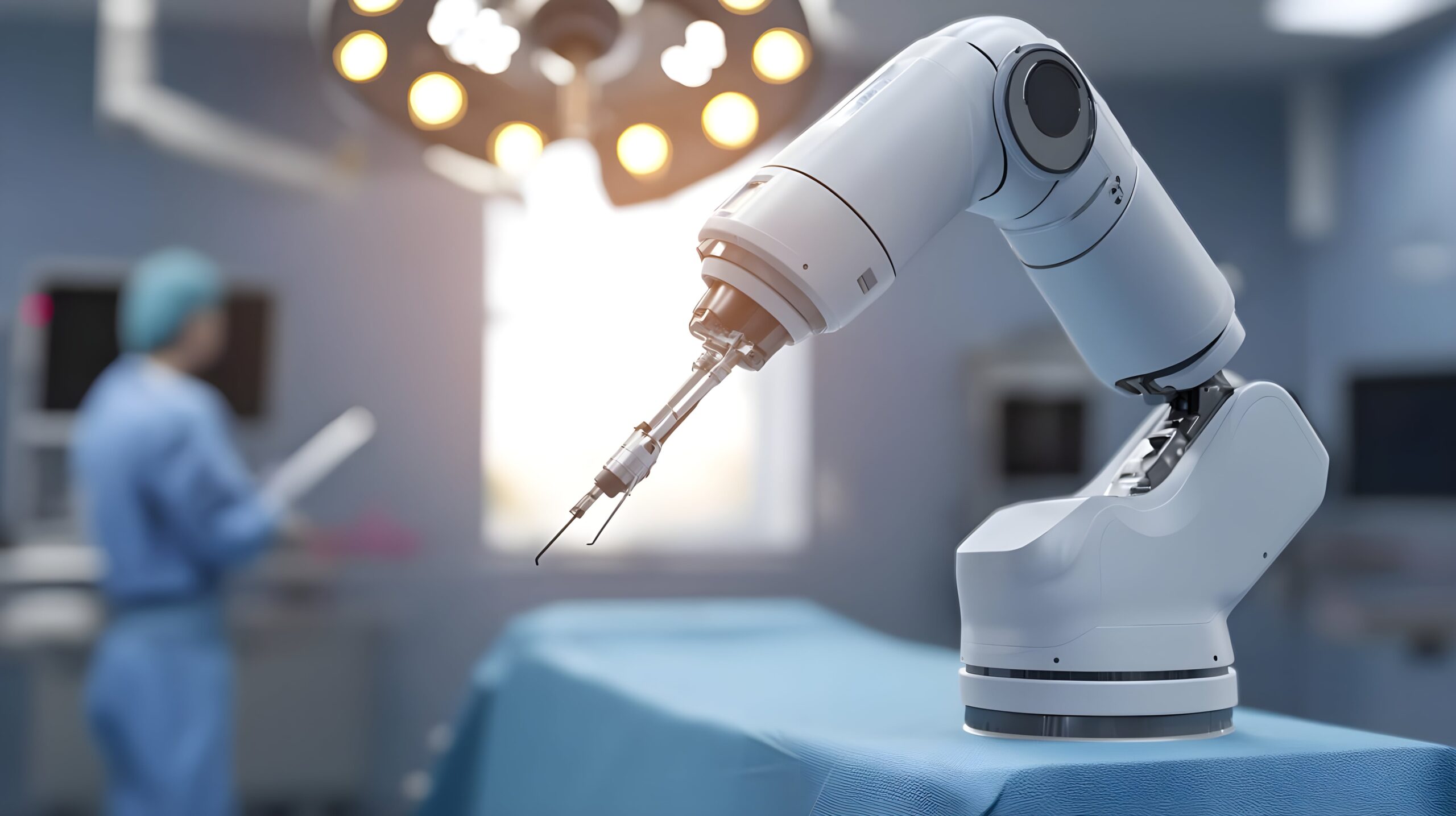
- Surgery: Procedures such as robotic radical prostatectomy involve removing the prostate gland. These are increasingly performed using advanced techniques like the da Vinci surgical system, which offers precision, minimal scarring, faster recovery, more certainty, and better preservation of backup (salvage) treatment options.
Exploring treatment pathways
Understanding the benefits and risks of each option is critical. For example:
- Robotic radical prostatectomy: This procedure is highly effective for localised cancer. With robotic assistance, surgeons can achieve exceptional precision, leading to better outcomes and quicker recovery times. Patients typically experience 1-2 day hospital stays and a rapid return to daily activities.
- Radiation therapy: Effective across various stages, radiation may require multiple sessions and may cause side effects such as fatigue or urinary symptoms. Choosing a clinic with the latest technology and experienced specialists can make a significant difference in treatment outcomes.
The timing of treatments is often critical. Early intervention – within weeks of diagnosis – can minimise disease progression and improve recovery outcomes. Open communication with your healthcare team is essential to establish a treatment plan that prioritises your health and well-being.
Coping with diagnosis and finding support
Emotional well-being
Receiving a prostate cancer diagnosis can feel like an emotional rollercoaster. It’s completely normal to experience anxiety, uncertainty, or even anger. These feelings are valid, and addressing them is an essential part of your journey. Seeking support from mental health professionals, such as counsellors or therapists, can help you process these emotions and develop coping strategies. Joining a support group can also be a powerful way to connect with others who understand what you’re going through.
Building a support network
No one should navigate this journey alone. Lean on family, friends, and support groups. In the UK, organisations like Prostate Cancer UK and Macmillan Cancer Support provide valuable resources, from helplines to peer support groups. Engaging with others who understand your experience can bring immense comfort and practical advice. Sharing your journey with loved ones can foster stronger relationships and provide the emotional support needed during treatment and recovery.
Empowering yourself through knowledge
Knowledge is empowering. Many patients feel more prepared with the more they know, and we are always here to offer advice. Take time to research treatment options, facilities, and specialists. Clinicians known for their expertise in prostate cancer care may offer cutting-edge treatment combined with compassionate support. Being informed equips you to make confident, well-rounded decisions. Understanding the latest advancements in prostate cancer treatment can also provide reassurance that effective options are available.
Life after diagnosis
Recovery and long-term outlook
Recovery largely depends on the cancer’s stage and the chosen treatment. For early-stage cancers, outcomes are often excellent, with minimal long-term effects. Regular follow-ups, including PSA tests and scans, are crucial to ensure any recurrence is caught early. Developing a follow-up care plan with your healthcare team can provide peace of mind and help you stay on track.
Living with advanced prostate cancer
For metastatic prostate cancer, the focus shifts to managing symptoms and maintaining quality of life. Treatments like hormone therapy and targeted therapies can slow the disease’s progression. Adjustments in diet, exercise, and stress management can also significantly enhance daily life. Many men find that staying active and maintaining a positive outlook helps them cope with the challenges of advanced cancer.
You’re not alone
A prostate cancer diagnosis marks the beginning of a journey – one that requires strength, informed decisions, and the support of loved ones and healthcare professionals. While the path may seem daunting, remember that advancements in medicine and supportive care offer hope at every stage. By staying informed, connecting with resources, and trusting in your care team, you can face this challenge with resilience and optimism. Every step forward, no matter how small, is a step toward better health and well-being.
For more information or to schedule a consultation, contact Santis Health.
If you have more questions about prostate cancer, such as hereditary risks or the latest treatment options, explore our article on 9 Common Questions About Prostate Cancer.

