The team at Santis Health are now approaching their 7th anniversary of regularly using NeuroSAFE – real-time, frozen-section analysis of the prostate during surgery to allow us to maximise nerve preservation without compromising on cancer control (i.e. removing the cancer). This is part of our drive to deliver better prostate cancer and functional outcomes for patients than have been possible in the past, and in this article, we’d like to share why we think it is an excellent development for patients.
Further research into this technique, documented in the Lancet Oncology journal, has shown marked improvements in retaining both post-operation erectile function as well as urinary continence. Through the NeuroSAFE PROOF trial, the study shows that men who had good erectile function before surgery were more likely to regain sexual function a year after their operation if the NeuroSAFE technique was used.
What is NeuroSAFE for prostate cancer?
NeuroSAFE stands for Neurovascular Structure Adjacent Frozen Section Examination. It is a technique that was first described by the Martini Klinik in Germany in 2014 that involves analysing the margins (edges) of a prostate immediately after it has been removed from a patient and whilst the surgery is still on-going to see whether cancer cells have reached the cut edge of the specimen. The prostate is delivered immediately to a pathologist in the room next door where it is frozen using a cryostat, cut into thin slices, stained with special dyes and examined under the microscope.
This analysis is done whilst the operation is still ongoing (the urethra has to be joined to the bladder after prostate removal), so it has to be done rapidly – typically within 20 minutes of the prostate being removed from the body. The team processing the tissue needs to work together quickly and efficiently to get the report to the surgeon within this time frame.
Why nerve-sparing matters in radical prostatectomy
To answer this question, let’s take a step back and consider nerve preservation for a moment. For most men, nerve-sparing is a key step during robotic radical prostatectomy and involves the preservation of the delicate nerves at the back of the prostate that control potency (erections). It is a technically demanding part of the operation and one where greater surgical experience has been shown to produce better results. Given the experience of the surgeons at Santis Health, it’s something that we are able to comfortably offer to the great majority of our patients.
However, in men in whom NeuroSAFE is not used with larger and/or more aggressive tumours that threaten the nerves around the prostate, the surgeon must make a choice during the operation between better cancer control (by removing the nerves) or better erections (saving the nerves but leaving open the possibility that cancer has in fact spread to them, causing problems later on). In these non-NeuroSAFE operations, the patient and surgeon must wait for the prostate to be sent to the pathology lab where it is dissected and analysed to produce the final pathology report on the severity of the cancer. This takes several days to be produced, meaning there is a considerable time lag between a surgeon’s reading of the prostate cancer and the scientific conclusion from the pathology lab. In this scenario, there can be no real-time interpretation of the tumour in the patient’s prostate.
The key question here is: are there cases in which we could spare the nerves if we knew decisively during the operation that the cancer had not spread outside the prostate? This is where NeuroSAFE comes in.
What is a positive surgical margin (PSM) and why does it matter?
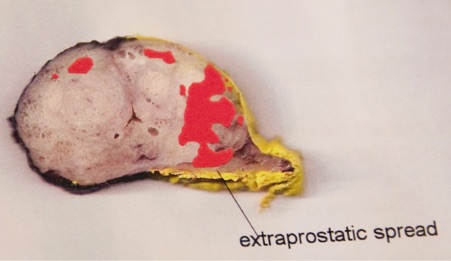
A positive surgical margin (PSM) means cancer cells are detected at the surface of the removed prostate tissue, indicating that some cancer may have been left behind. Pathologists identify a PSM by applying ink to the surface of the prostate specimen; if cancer cells are in contact with this ink, the margin is considered positive. In the example below (black ink for the left side, yellow ink for the right), negative, or clear, surgical margins were achieved all around the prostate, meaning no cancer cells touched the ink.
PSMs increase the risk of cancer recurrence, with the likelihood typically ranging from 5% to 20%, depending on the aggressiveness of the cancer.
Avoiding PSMs is a key goal in any prostatectomy, and NeuroSAFE techniques help surgeons achieve this goal while still attempting to preserve the surrounding nerves wherever safely possible.
Benefits of the NeuroSAFE prostatectomy technique
NeuroSAFE benefits patients in several important ways:
Better nerve preservation without sacrificing cancer control
Surgeons can preserve one or both neurovascular bundles with greater confidence, even in borderline cases, knowing they have real-time feedback from pathology.
Improved erectile function outcomes
Evidence shows that men who undergo radical prostatectomy with NeuroSAFE have a higher chance of recovering sexual function. The NeuroSAFE PROOF trial, published in Lancet Oncology in 2025, found that 32% of men in the NeuroSAFE group regained erections sufficient for intercourse after 12 months, compared with just 18% in the standard surgery group.
No increase in cancer recurrence
Crucially, the same trial also confirmed that using NeuroSAFE does not increase the risk of leaving cancer behind. There was no significant difference in positive surgical margins (27% in the NeuroSAFE group vs 25% in the control group) or PSA recurrence rates at 12 months.
More informed surgical decision-making
The trial also showed that surgeons were more likely to attempt and succeed at bilateral nerve-sparing with NeuroSAFE (76% attempted vs 45%; 63% successful vs 32%).
Maintained urinary continence outcomes
While the primary benefit of NeuroSAFE is improved sexual function, continence rates were comparable across both groups.
Real-time intraoperative assurance
With the NeuroSAFE technique, it allows for faster, evidence-based decisions during surgery, removing the need to wait several days for final pathology results.
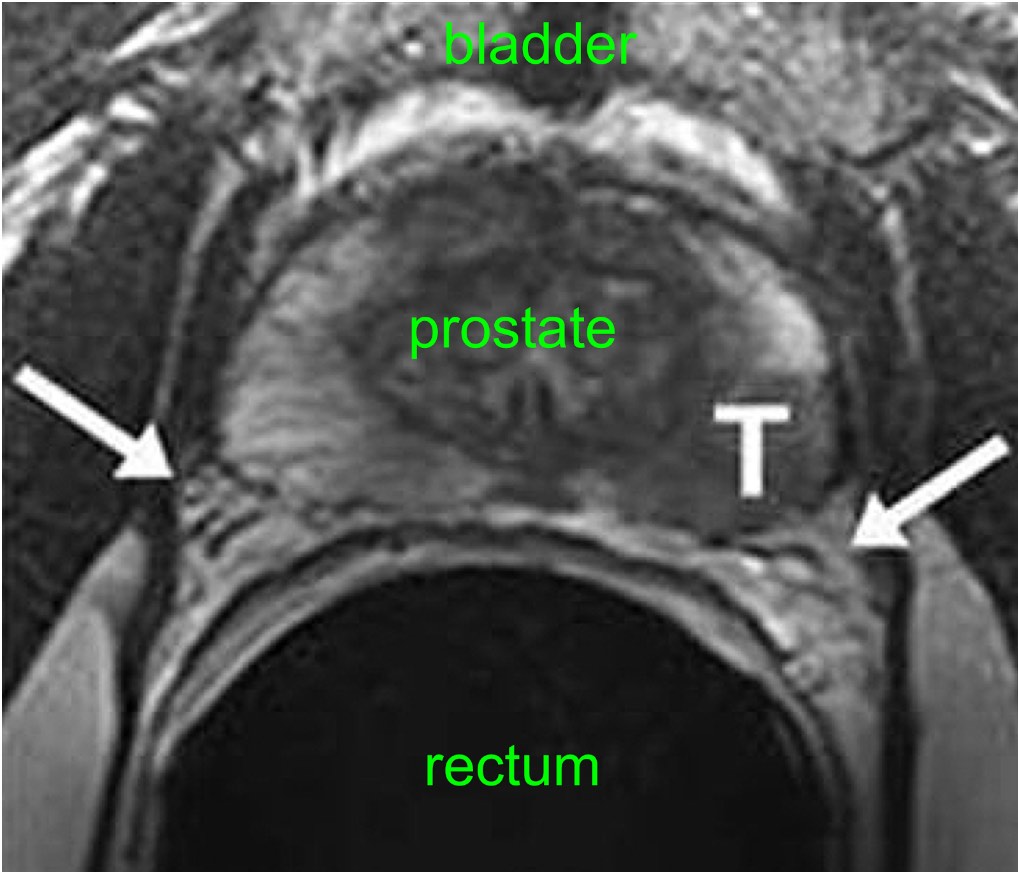
The 2 nerves of potency are identified by the 2 white arrows on this MRI scan. The left nerve lies very close to the tumour (‘T’). This is a common situation and one in which the NeuroSAFE technique would allow the surgeon to achieve both optimal cancer control and optimal functional results.
Why choose Santis for your radical prostatectomy with NeuroSAFE?
At Santis, our surgeons are among the UK’s most experienced in robotic prostatectomy and nerve-sparing procedures. By combining expertise with advanced techniques like NeuroSAFE, we aim to offer our patients the best possible outcomes.
We have implemented NeuroSAFE at London Bridge Hospital, where it is supported by skilled pathology teams that can provide rapid intraoperative analysis. Our results align with the international evidence: improved nerve preservation, high cancer control, and better patient outcomes.
Want to learn more about whether NeuroSAFE is right for you?
Explore our dedicated pages on Nerve-Sparing Prostate Surgery, Robotic Prostatectomy, and Screening & Diagnosis to learn more about our approach.
Or contact us directly to speak to one of our specialists or book a consultation.
FAQs: NeuroSAFE and prostate cancer surgery
What is NeuroSAFE?
NeuroSAFE is a surgical technique that provides real-time pathological analysis of prostate tissue margins during radical prostatectomy, helping surgeons more safely and frequently preserve the nerves responsible for potency.
Is NeuroSAFE available in all hospitals?
No. The technique requires an on-site pathology team and rapid tissue-processing infrastructure, making it more suited to high-volume specialist centres. Santis Health offers NeuroSAFE at London Bridge Hospital.
Does NeuroSAFE improve outcomes?
Yes. The NeuroSAFE PROOF trial showed improved erectile function without increasing cancer recurrence risk. It also increased the rates of successful bilateral nerve-sparing.
Does NeuroSAFE affect continence outcomes?
No. Studies have shown continence outcomes remain the same between NeuroSAFE and non-NeuroSAFE groups.

