One of the commonest concerns voiced by patients contemplating having prostate cancer surgery is the prospect of having a catheter inserted in the penis for 1-2 weeks after the operation to drain urine while your bladder is healing from the operation. In this article I explain why this should not be something to fear, and explain more about how we urologists use catheters.
How does a catheter work?
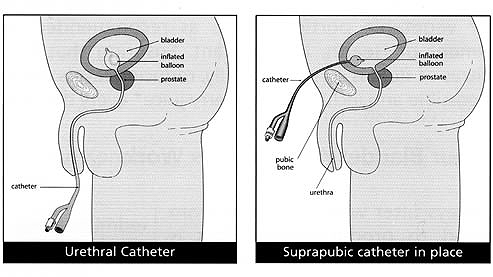
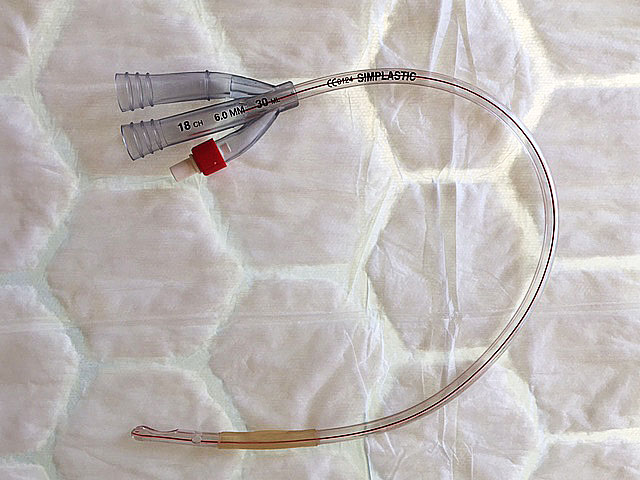
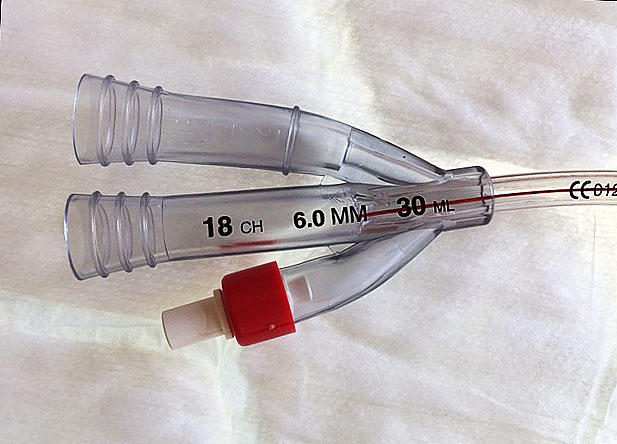
A catheter is simply a hollow plastic tube that is used to drain urine from the bladder. There is a balloon on the end which stops it from falling out of the bladder, and this is inflated with sterile water or deflated via the balloon inflation port.
A catheter is normally inserted into the bladder via the urethra (the tube that drains urine to the outside world) – this is known as a urethral catheter. Alternatively, the catheter can also be inserted under anaesthetic through the lower abdomen – this is known as a suprapubic catheter. A suprapubic catheter is normally inserted following a Retzius-sparing prostatectomy.
The advantages of a suprapubic catheter
- It is more comfortable – this has been confirmed by a study published in 2009 in European Urology;
- It has a lower urine infection rate – as confirmed in 2006 in the British Journal of Surgery;
- It is easier for patients to manage – the ‘trial of voiding’ (testing to see whether normal bladder function has returned following prostate removal) can be done at home by turning the Flip-Flo valve (see below) to the closed position. This allows the bladder to fill and the patient to pass urine through the normal route. Patients then attend hospital the following day just to have the catheter removed and a dressing applied. If a patient can’t pass urine normally during the trial of voiding, the Flip-Flo valve can simply be opened to drain the bladder rather than having to re-insert a catheter which is the case when a urethral catheter has been used.
- The catheter can be removed sooner – the catheter can be removed (typically 8 days) earlier than a urethral catheter.
What are the various components?
Catheter drainage bags
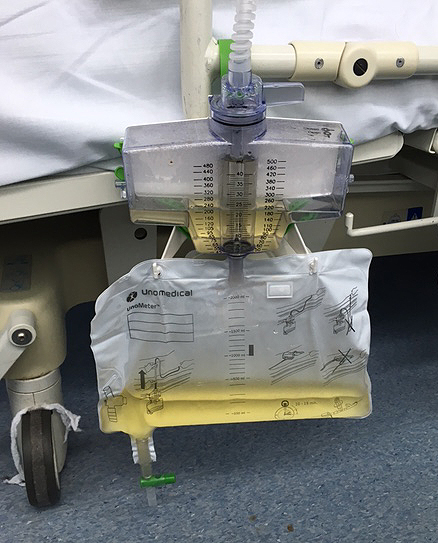
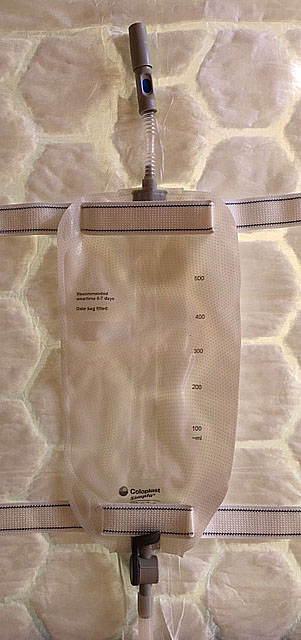
A large bag is connected to the catheter after the operation, which allows the urine output to be measured hourly to ensure that it is draining correctly. On the first morning after the operation this will be changed to a leg bag, which is attached to the thigh inside the patient’s trousers and which is smaller in capacity. At night, the leg bag is connected to a larger night bag so that patients don’t have to get out of bed to empty the smaller leg bag every 3-4 hours.
Flip-Flo valve
This is simply a switch between the suprapubic catheter (if used) and the catheter drainage bag that either allows urine to flow through it (in the open position) into the drainage bag or not (in the closed position), where urine flows out through the penis. It should always be open except during the trial of voiding.


Catheter types
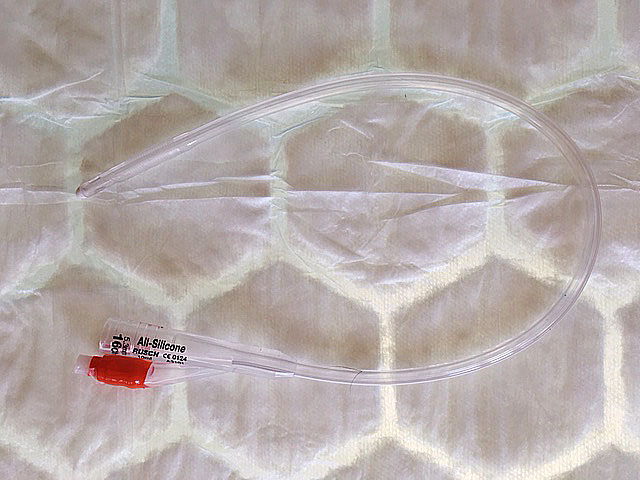
A 2-way (one balloon inflation channel + a urine drainage channel) catheter is used after radical prostatectomy. A 3-way catheter includes a channel for irrigation fluid to run into the bladder and is used following transurethral prostate surgery (for an obstructing, rather than a cancerous, prostate) and not following radical prostatectomy.
Catheter materials
A silicone catheter, which is soft and inert, is used after radical prostatectomy. Stiffer (Simplastic 3-way catheters are used following transurethral prostate surgery but not following radical prostatectomy).
Catheter sizes
These are measured in Charriere (Ch) or French (F) units and relate to the circumference of the catheter in millimetres (mm). The most commonly used size of catheter after radical prostatectomy is 16F, which is 16/pi = 5 mm in diameter.
Catheter removal
This is easily done a few weeks after surgery by deflating the balloon on the end of the catheter and gently withdrawing it. A dressing is applied to the suprapubic catheter site and the opening closes within a few minutes.
Learn more about post-operative care or book a consultation with the Santis team to discuss your prostate cancer treatment options.

