Introduction
As enlightened readers of the Prostate Cancer Information Centre will know by now, the PSA test on its own cannot tell us if a patient has prostate cancer (many patients with prostate cancer in fact do not have an abnormal PSA level) – it is only an indicator, although generally a reliable one. As a result, further investigation is required. This involves tests in the form of an MRI scan and/or a biopsy, which are performed to give the urologist a much clearer picture and firm data about any possible cancer.
An MRI scan on its own isn’t good enough though. Although MRI scanning is getting close to being able to reliably predict the presence of a significant (Gleason grade 7 or higher) prostate cancer, it is still only 80% accurate. We can’t therefore rely on it on its own. Only prostate cancer seen under a microscope by a trained pathologist can be taken as incontrovertible proof of the presence of cancer within a prostate gland, and this requires a biopsy to be performed. Now, there are two methods of performing a biopsy, and I’d like to explain the differences between the two so that patients fully understand the process and can ask their urologist which one will be performed.
Transrectal prostate biopsy method
Prostate biopsy has traditionally been done via the transrectal route – i.e. via the rectum. This is because before the advent of transrectal ultrasound (where an ultrasound probe is placed in the rectum to provide a visual of the prostate as the needles were inserted into it), the biopsies were finger-guided. This means that the biopsy needle was placed alongside a gloved finger placed in the rectum, which allowed the operator to feel which part of the prostate to guide the needle into. The advent of the transrectal ultrasound probe allowed urologists to see exactly where the needle was within the prostate before the biopsy was taken, allowing a much greater degree of accuracy than with the finger-guided approach.
However, even with the probe to help problems remain with transrectal prostate biopsies. These include:
- An infection rate of 10-20% due to needles penetrating the rectal wall, and faecal matter contaminating other parts of the body.
- A serious infection (septicaemia or blood poisoning) rate of 1-2%.
- The development of antibiotic-resistant strains of bacteria causing infection.
- Pain during biopsy.
- Inability to accurately place the biopsy needle within the prostate in 3 dimensions.
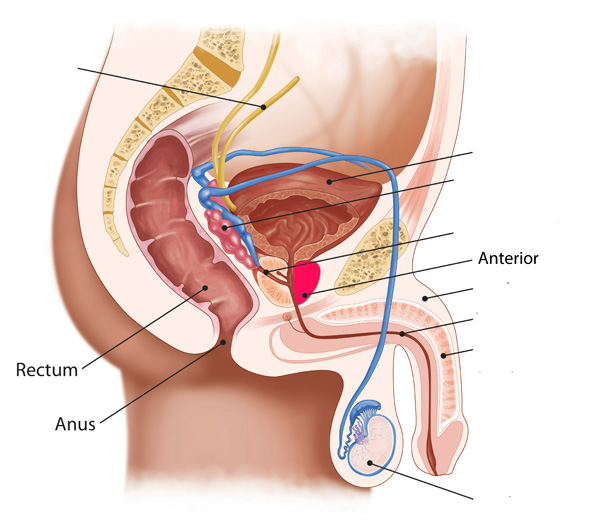
In addition, perhaps the biggest downside of the transrectal approach is that it is harder/impossible to reach the part of the prostate (the anterior, or frontal aspect) that is furthest away from the biopsy needle. This leads to poor ‘sampling’ – in that the tissue samples collected by the needles may miss any cancer found in this part of the prostate, leading to an inaccurate biopsy. Playing devil’s advocate, you could imagine that in a worst-case scenario cancer is present in the anterior portion while no cancer is present in the other parts of the prostate. A transrectal approach might miss the cancer in the anterior, with the biopsy coming back clear from the other parts of the prostate. In essence, all parts of the prostate need to be sampled completely for the most accurate biopsy result.
Transperineal prostate biopsy method
The answer to the above problems lies in using a transperineal approach to inserting the needles – meaning that the needles go through the perineum (the area behind the scrotum and in front of the anus) instead of through the rectum. A brachytherapy grid is placed over the perineum to allow accurate placement of the biopsy needle within the prostate, together with the use of an ultrasound probe to direct the urologist. This allows better sampling of all parts of the prostate, including the anterior section. Compare the two images below showing a transrectal approach first and a transperineal approach second, and notice how the transperineal approach allows us better access to all parts of the prostate.
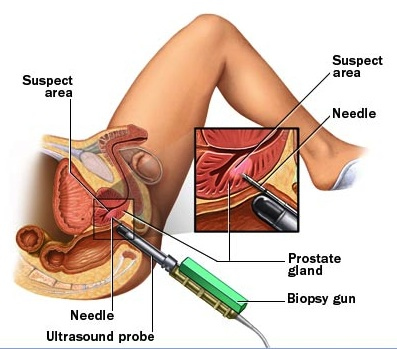
Transrectal prostate biopsy
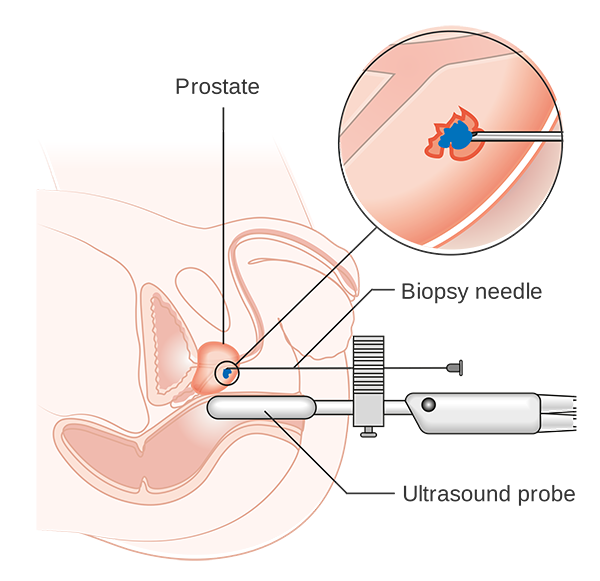
Transperineal prostate biopsy
Targeting the biopsy accurately using MRI
By doing an MRI scan before a transperineal prostate biopsy (which is my general practice for patients), we can identify the suspicious areas to be specifically targeted during the biopsy – increasing the accuracy of the biopsy. This can either be done by comparing the MRI scan with the transrectal ultrasound view during the biopsy process (cognitive targeting) or by overlaying the 2 images in real-time using computer software: fusion biopsy. Because patients are asleep under a general anaesthetic for transperineal biopsy, discomfort during the biopsy process is not an issue, allowing many more samples to be taken and so increasing the detection rate. And because the biopsies are not taken via the rectum, infection-related complications are much less common.
In summary
The point of a biopsy is to accurately determine the grade of prostate cancer, and so we must be able to access the whole of the prostate to do so. A quick overview of the main points of comparison is found below.
| Transrectal | Transperineal | |
|---|---|---|
| Anaesthetic | Local | General |
| Hospital stay | Outpatient | Day case |
| Discomfort during procedure | Moderate | None |
| Discomfort after procedure | Ache | Ache |
| Infection risk | 10-20% | 1-2% |
| Serious infection (septicaemia) risk | 1-2% | Less than 1% |
| Ability to sample anterior prostate | Limited | Full |
| Allows systematic sampling (prostate mapping) | No | Yes |
Have questions about prostate biopsies or your next steps?
Our team is here to provide guidance and support. Contact us for more information or to book a consultation with one of our specialists.

