Introduction
Occasionally I have patients coming to see me to enquire about surgery after HIFU treatment has not cured their cancer completely. In some cases, it comes back quite aggressively, so I wanted to write this article to explain what can be done for such patients and what the prognosis can be.
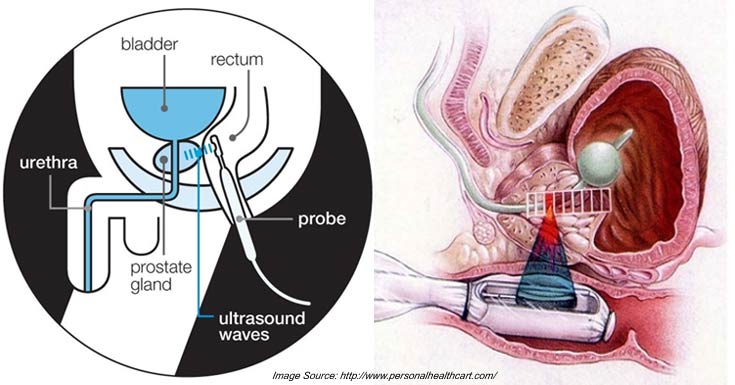
How HIFU works
For those who are unfamiliar with the technique, High Intensity Focused Ultrasound (HIFU) is a way of treating prostate cancer that is less invasive than surgery. The technology behind it was actually developed shortly after the Second World War by the aviation industry to remove debris from the leading edge of aircraft wings to ensure that they continued to work efficiently after they left the factory.
When applied to areas of the human body (i.e. the cancerous areas we want to treat), the high frequency ultrasound waves causes the body tissues to heat up to very high temperatures, killing the cells. This effect was used to treat benign prostate enlargement in the 1990s, but never gained acceptance because there are faster alternatives, such as transurethral resection of the prostate (TURP). HIFU started to be used in Europe to treat prostate cancer in the 2000s – patients became attracted to the technique because it was less invasive than surgery and promised fewer side effects than surgery or radiotherapy – the thinking being that if only part of your prostate had cancer, there was no reason to treat all of it.
HIFU treatment diagram
More than a decade on from HIFU’s launch, we now have medium-term data that demonstrate that it is a safe treatment in the main (no treatment is entirely complication free), but is not as effective as radiotherapy or surgery in controlling prostate cancer where the whole prostate is treated.
Most of the current interest in HIFU is therefore in its use for focal therapy, typically to treat only one side of the prostate in men with prostate cancer that has been discovered only in that one side. The aim of treating only part of the prostate is to minimise side-effects, but leaves the potential disadvantage that it may not be as effective in controlling cancer if some areas or cells are missed. This remains to be either proven or disproven in clinical studies and trials, however.
Surgery after HIFU
When HIFU fails and the cancer returns/spreads, surgery and radiotherapy become the main options as the focus shifts to providing a final cure. Just to make clear, surgery is still possible for ex-HIFU patients, although the operation needs to be done by an experienced surgeon because of the greater technical difficulty due to scarring around the prostate. We call such an operation a salvage prostatectomy. Indeed, because the tissue destruction caused by HIFU is so localised, salvage prostatectomy is in general easier than after radiotherapy (including external beam radiotherapy and brachytherapy) – both of which cause a lot of scarring around the prostate. My results show that this easier dissection appears to translate into a much lower complication rate and much better functional results (i.e. for continence and potency) than after salvage surgery following failed radiotherapy. If your HIFU treatment has failed – do not give up hope – surgery may still offer a permanent cure for you with very good functional results!

Success stories
Several patients have reported permanent cure of their cancer after they came to me following unsuccessful HIFU treatment. Here are some of their profiles:
- G.K., age 65 years at time of surgery, Gleason 3+4, stage T2c, unrecordable PSA at last follow-up at 2.5 years following surgery. He remains both continent and potent.
- W. W., age 61 years, Gleason 3+4, stage T2a, unrecordable PSA at last follow-up 9 months following surgery. He remains both continent and potent.
- M. P., age 63 years, Gleason 3+4, stage T2a, unrecordable PSA at last follow-up 6 months following surgery. He remains continent, but experienced erectile dysfunction before surgery and so was not potent after surgery.
Outcomes after surgery
However, it’s important to say that the ultimate outcome after surgery in terms of cancer control still depends on the characteristics (extent and grade) of the cancer before the HIFU and the characteristics, amount and location of the remaining cancer following HIFU. These can be determined by prostate biopsy, multiparametric MRI scan and bone scan. The main risk for HIFU patients is the time delay involved compared with patients who just opt for surgery straight away as their first treatment – if the cancer has spread since HIFU treatment, then it may complicate things.
Ongoing research
As it happens, I am one of the surgeons involved in the RAFT study – Robotic surgery After Focal ablation Therapy – and am including my patients in it if they consent. As its name suggests, the aim of this UK-based study is to investigate and quantify the effects of prior focal therapy (usually HIFU) on the success of salvage robotic radical prostatectomy.
Participation in the study is not mandatory for patients considering salvage surgery after HIFU, but my aim is to work to build the body of evidence to confirm initial findings that surgery is a safe, effective and well-tolerated way to manage patients who have failed HIFU. I’ll be sharing my findings with you over the coming months and years.